 The U.S. healthcare system is currently characterized by increasing fragmentation, where patients, in a move to cut costs and maintain convenience, now exhibit a fleeting loyalty to prescription products and a distant relationship with physicians.
The U.S. healthcare system is currently characterized by increasing fragmentation, where patients, in a move to cut costs and maintain convenience, now exhibit a fleeting loyalty to prescription products and a distant relationship with physicians.
This was one of the key insights gleaned by findings in a recent national survey conducted by New York-based independent agency Finn Partners, which gauged the attitudes and behaviors of patients navigating today’s healthcare landscape.
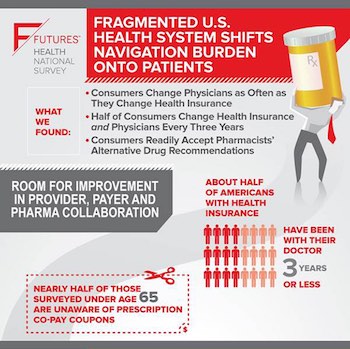
The Finn Futures survey shows that current insurance formularies and out-of-pocket costs could be influencing more consumer healthcare decisions than ever. Most Americans — 51 percent — now change their insurance plans at least every three years, and a similar number of consumers with health insurance — 45 percent — now keep their primary care physician for only the same amount of time, even though respondents said they still regard their doctor as the single most trusted source of health information. Almost half of those polled — 46 percent — said they visit their primary care physician only once a year, though 55 percent now said they avoid a doctor’s office altogether.
“For many people, there’s no such thing as a primary care physician any more,” Gil Bashe, managing partner of Finn Partners' health practice, told O’Dwyer’s. “That means there's no central place where a record of our health information resides. One problem we’re going to see is that more people’s health concerns are not managed sooner because, in much the same way that the healthcare system has become fragmented, our personal health information has become fragmented as well.”
Cost and convenience also prove increasing factors in determining what medicines patients now opt to buy. While a majority of respondents — three out of four — said they consult with either their doctor or pharmacist if they have questions about a prescription, the survey found that 43 percent of consumers now receive pharmacists’ recommendations regarding alternatives to medications prescribed by their doctor, and nearly half of all respondents said they take their pharmacist's advice on those cost-effective alternatives.
Left to navigate the system without the regular guidance of a doctor or long-term insurers, patients and consumers arguably wield a diminished voice in today's healthcare landscape. For this reason, Bashe said the onus is on leaders in the pharmaceutical, policy and provider sectors to make collaborative strides in showcasing the value of healthcare services and products for patients. Improved communication efforts are paramount.
“The data should cause everyone to step back and see where things are going from a communications standpoint,” Bashe said. “These sectors have to realize that they're not competing here, they’re part of a collaborate resource, and they need to invite the consumer to participate in being part of that dynamic. As communicators, our job has always been to connect people with a common call to action."
Indeed, the survey indicated that education could play a major role in influencing consumer healthcare behavior. Nearly half of respondents in the Finn Futures survey said they were unaware that pharmaceutical companies offer co-pay cost-saving options for prescription medicine, such as savings cards, which aid the burden of out-of-pocket expenses. Only eight percent admitted visiting a medication's website.
“The biggest challenge for health insurance companies and providers is that many American consumers don't understand how the system works. They access the system only when they have a problem,” Bashe said. “We've got to make the practice of seeing a doctor something important.”
The Finn Futures survey was conducted in November and polled 1,000 U.S. residents online. It was led by research director Christopher Lawrence, in Finn Partners' Washington, D.C. office. The data will be presented globally next week, at the annual mHealth Israel conference in Tel Aviv.
Detailed results of the survey’s findings can be found here.

 Lo Isidro, senior director at Real Chemistry with more than a decade of strategic communications and PA experience, has joined Narrative Strategies.
Lo Isidro, senior director at Real Chemistry with more than a decade of strategic communications and PA experience, has joined Narrative Strategies. Nelson Fernandez, former North American chair of APCO Worldwide and managing director of Burson-Marsteller, has joined Volunteers in Medicine Berkshires as director of communications and PA.
Nelson Fernandez, former North American chair of APCO Worldwide and managing director of Burson-Marsteller, has joined Volunteers in Medicine Berkshires as director of communications and PA. Lilit Bargar, who was most recently an EVP in the healthcare practice at Weber Shandwick, comes on board at GCI Health as EVP, corporate practice lead.
Lilit Bargar, who was most recently an EVP in the healthcare practice at Weber Shandwick, comes on board at GCI Health as EVP, corporate practice lead.
 Five ways that successful thought leaders are made.
Five ways that successful thought leaders are made.


 Have a comment? Send it to
Have a comment? Send it to 
No comments have been submitted for this story yet.